Table of Contents
ToggleAn abnormal growth or division of cells in the pancreas leads to pancreatic cancer. Located near the spine, the pancreas produces digestive enzymes deep in the abdomen. By producing enzymes and hormones, it aids digestion and controls blood sugar levels. The pancreas is composed of cells. A cell divides when it is needed to create a new one. As cells age, they die and are replaced by new ones. This process can fail sometimes.
Whenever the body does not need new cells, or old cells are not destroyed, new cells are formed. As a result of the extra cells, a tumor may develop. Tumors can be benign. Their abnormality does not allow them to invade other parts of the body. It is called cancer when the tumor is malignant. This can lead to the cells growing out of control and spreading to other organs and tissues. Cancer that starts in the pancreas can still be called pancreatic cancer even after it has spread to another part of the body. There are several organs where pancreatic cancer can spread, including the liver, abdomen wall, lungs, bones, and lymph nodes.
Causes of Pancreatic Cancer:
Cancer is caused by changes in the DNA of your body. Parents can pass on these traits to their children or they can develop over time. You can develop changes over time if you’ve been exposed to something harmful. It is also possible for them to occur at random. It is unclear what causes pancreatic cancer. The majority of pancreatic cancers are hereditary or familial. Smoking, obesity, and aging are the main causes of pancreatic cancer.
You may be more likely to develop pancreatic cancer if you have a first-degree relative with the disease. When a family member has pancreatic cancer, genetic testing is strongly recommended. Genetic testing is often not necessary if your results are negative.
Types of Pancreatic Cancer:
Pancreatic cancer comes in many forms, but exocrine cancer is the most common. You are likely to have exocrine pancreatic cancer if you have been diagnosed with pancreatic cancer.
Pancreatic adenocarcinoma:
In about 95% of cases, exocrine pancreatic cancer is an adenocarcinoma. Pancreatic cancer usually starts in the ducts of the pancreas. They are called acinar cell carcinomas when they arise from the cells that produce pancreatic enzymes.
Less common exocrine cancer:
These cancers are less common than those caused by exocrine hormones, including adenosquamous carcinomas, squamous cell carcinomas, signet ring cell carcinomas, and undifferentiated carcinomas.
Ampullary cancer:
A bile duct, pancreatic duct, and small intestine duct form the ampulla of Vater, which is where this cancer begins. The treatment for ampullary cancer is similar to that for pancreatic cancer, although they aren’t technically pancreatic cancers. Ampullary cancer often blocks the bile duct when it is still small and has not spread much.
Major Symptoms of Pancreatic Cancer:
Some pancreatic cancers don’t have symptoms, or they are hard to detect. It can cause the following symptoms: Your skin may also become itchy, your pee may be darker, and your poo may be paler than usual Unintentional weight loss or loss of appetite Having no energy or feeling tired Having a high temperature or feeling hot and shivering. You may also experience digestive problems if you have any of the following symptoms:
Sickness or feeling unwell Constipation or diarrhea, or other changes in your bowel movements You may experience pain in your tummy and back when you’re eating or lying down, but it may go away when you lean forward Indigestion symptoms, such as feeling bloated.
Consumption of tobacco:
The risk of pancreatic cancer is greatly increased by smoking. As compared to people who don’t smoke, people who smoke have about twice the risk of developing this cancer. It is believed that approximately 25% of pancreatic cancer cases are caused by cigarette smoking. The risks are also increased by smoking cigarettes and using smokeless tobacco products. As soon as a person stops smoking, their risk of pancreatic cancer decreases.
Risk Factors to Look After for Pancreatic Cancer:
Any factor that increases your chances of contracting a disease, such as cancer, is a risk factor. There are different risk factors for different types of cancer. There is no guarantee that you will get cancer just because you have a risk factor. People may not be aware of the factors that contribute to cancer risk. The following factors increase the risk of pancreatic cancer.
Obesity:
Pancreatic cancer is associated with being very overweight. The risk of pancreatic cancer is about 20% higher for obese individuals. The risk of developing diabetes can also be increased by gaining weight as an adult. People who are not very overweight may also be at risk of carrying excess weight around the waistline.
Diabetes:
People with diabetes are more likely to develop pancreatic cancer. There is no explanation for this. Type 2 diabetics are at the greatest risk. In children and adolescents, these types of diabetes are on the rise as obesity also increases in these groups. Being overweight and obese are also associated with type 2 diabetes in adults. Type 1 diabetes is not known to be riskier.
Chronic pancreatitis:
It is known that chronic pancreatitis, an inflammation of the pancreas over a long period, increases the risk of pancreatic cancer. As a result of heavy alcohol consumption and smoking, chronic pancreatitis often develops.
Chemical exposure in the workplace:
People who work in the dry cleaning and metal working industries may be more likely to develop pancreatic cancer if they are exposed to certain chemicals at work.
Diagnosis of Pancreatic Cancer:
To determine the cause of pancreatic cancer signs and symptoms, certain exams and tests will be conducted. The extent of cancer will be determined through further tests if cancer is detected.
Medical history and physical exam:
Your doctor needs to know your medical history to understand your symptoms. Smoking and your family history may also be asked about by your doctor. As part of your examination, your doctor will look for signs of this cancer or other health problems. Doctors might be able to feel swelling in the liver or gallbladder during an exam when pancreatic cancer is present. Jaundice will also be checked on your skin and eyes.
Imaging tests:
Radioactive substances or x-rays are used in imaging tests to create pictures of what’s inside the body. Before and after a pancreatic cancer diagnosis, imaging tests could be done for a variety of reasons, including To detect suspicious areas that might be cancerous Find out how far cancer has spread Assess the effectiveness of treatment Detect recurrence of cancer after treatment.
Blood tests:
If pancreatic cancer is detected, blood tests can help determine its treatment options, as well as diagnose it.
Liver function tests, Tumor markers, and Other blood tests.
Biopsy:
The diagnosis of pancreatic cancer can only be confirmed by removing and studying a small sample of the tumor under a microscope, even if a person has a medical history, physical exam, and imaging test results suggesting it. It is known as a biopsy. It is possible to perform biopsies in different ways.
Percutaneous, biopsy Endoscopic, and biopsy Surgical biopsy.
Stages of Pancreatic Cancer:
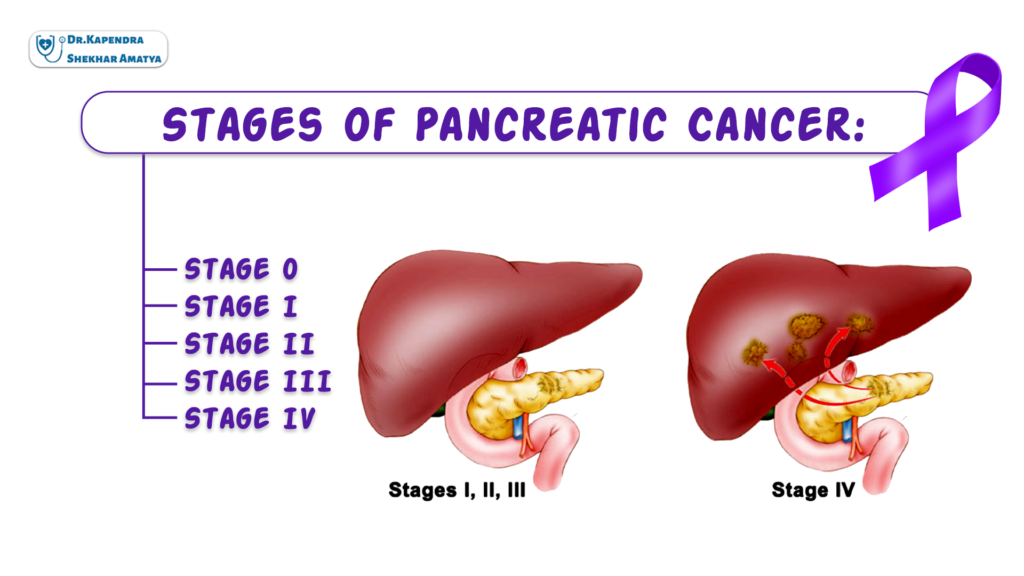
Depending on the size and extent of the metastasis, pancreatic cancer is staged. According to the results of various tests and exams, pancreatic tumors can be staged.
Stage 0:
In the lining of the pancreas, abnormal cells are found. A cancerous cell may spread to nearby normal tissue and be metastatic. Cancer in situ is also known as stage 0.
Stage 1:
The pancreas is the only organ that can develop cancer. Depending on the size of the tumor, stage 1 is divided into the following stages: Tumors with a diameter of two centimeters or less and Tumor size exceeding 2 centimeters.
Stage 2:
In addition to metastasizing to nearby tissue and organs, cancer may have spread to lymph nodes near the pancreas as well. Based on where cancer has spread, stage II is divided into the following stages: In nearby tissues and organs, there are signs of cancer, but it has not spread to lymph nodes, major blood vessels, nerves, or distant parts of the body. It has spread to nearby lymph nodes and may have spread to nearby tissue and organs. However, cancer has not spread to distant sites or major blood vessels or nerves.
Stage 3:
A major blood vessel near the pancreas has been affected with cancer, and lymph nodes may also have been affected. No other locations have reported it spreading.
Stage 4:
There is no limit to the size of cancer, and it can spread to distant organs like the liver, the lungs, and the peritoneum. Also, lymph nodes and organs near the pancreas may be affected.
Treatment of Pancreatic Cancer:
Early detection of pancreatic cancer increases the likelihood of successful treatment. In addition to treatments that can help control late-stage of this cancer, it may also be possible to help patients live longer.
Surgery:
According to the location and size of the tumor in the pancreas, surgery for pancreatic cancer involves removing all or part of the pancreas. In addition to the tumor, healthy tissue is often removed around it. Margin refers to this. When healthy tissue is removed from the margins, the goal is to have clear margins, which means there are no cancer cells there.
Radiation therapy:
High-energy particles or x-rays are used in radiation therapy to kill cancer cells. Radiation oncologists specialize in treating cancer with radiation therapy. Radiation from a machine outside the body is the most common type of radiation treatment.
Chemotherapy:
It is a method of destroying cancer cells by preventing them from multiplying, dividing, and producing new ones. In chemotherapy regimens, cycles are given over a set period; each cycle is called a cycle. Cycles are usually separated by rest periods. Several drugs may be administered at the same time to a patient or one drug may be given at a time along with another.
Targeted therapy:
An intervention targeting specific genes, proteins, or cell environments that contribute to the growth and survival of cancer is called targeted therapy. Cancer cells cannot grow or spread under this type of treatment, and healthy cells are less likely to be damaged. Tumors have different targets. Testing your tumor’s genes, proteins, and other factors can help your doctor determine the best treatment. As a result, doctors can identify the most effective treatment for each patient.
Immunotherapy:
It is a method of fighting cancer that boosts the body’s natural defenses by stimulating the immune system. Materials produced in the body or a laboratory are used to improve, target, or restore immune system function. As part of emerging clinical trials, immunotherapy is also being studied in conjunction with chemotherapy. It is possible to experience different side effects from different types of immunotherapy.
When to See an Oncologist in Nepal?
It is best suggested to see a cancer specialist when you observe any of the symptoms of pancreatic cancer. For this, you can either go for a surgical oncologist or a medical oncologist. As per the top surgical oncologist in Nepal Dr. Kapendra Shekhar Amatya, it is best to consult your cancer doctor as soon as possible rather than staying at home and trying to cure it on your own.

MS (NMC Regd.2902)
Head of the Department, Sr.Consultant Surgical Oncologist at Nepal Cancer Hospital and Research Center
Director: Breast Cancer Program
Interest: Breast Cancer Surgery, Gastro Intestinal Cancer Surgery (Stomach and Colo-Rectal Cancer)