Table of Contents
ToggleA lumpectomy surgery involves removing cancerous or abnormal tissue from your breasts. An initial lumpectomy removes a small amount of healthy tissue surrounding the cancer or other abnormality. Having all the abnormal tissue removed in this way ensures that it is completely removed.
Early-stage breast cancer can be treated with lumpectomy. It is sometimes used to rule out cancer after a lumpectomy. To reduce the chances of cancer returning after lumpectomy surgery, radiation therapy is usually administered to the breast.
Who Should Go for Lumpectomy?
A lumpectomy may be right for you if:
• Your breast is only affected by cancer in one area.
• When compared to the size of your breast, a tumor is relatively small
• It is expected that you will have enough remaining tissue after your tumor has been removed to reshape your breast.
• Radiation treatment can be completed.
When Should You Not Choose Lumpectomy as an Option?
Several factors may prevent your healthcare provider from recommending a lumpectomy. Large cancer or multiple tumors in one breast may prevent you from undergoing this procedure. A lumpectomy is usually followed by radiation therapy. In the case that your provider doesn’t recommend radiation therapy or you do not wish to have radiation, a lumpectomy might not be a good option for you. In cases where you previously received radiation therapy in the same breast or are pregnant, your provider may recommend avoiding radiation.
A lumpectomy and radiation may also be avoided if you have:
• An increase in your risk of getting breast cancer again due to a genetic mutation
• An inflammatory breast cancer
• Radiation therapy side effects may be more severe if you suffer from Lupus or another medical condition.
Why Should You Choose Lumpectomy Over Other Procedures?
The purpose of a lumpectomy is to remove cancerous tissue from your breast while protecting its appearance. For early-stage breast cancer, a lumpectomy followed by radiation therapy is as effective as removing the entire breast (mastectomy). If a biopsy shows that you have cancer, and if the cancer is small and in its early stages, your doctor may recommend a lumpectomy. A lumpectomy may also be used to remove abnormalities of the breast that are not cancerous or precancerous.
Is it Effective to Get Radiation after Surgery?
Radiation treatments are usually performed after lumpectomy surgery to eliminate any remaining microscopic cancer cells. Breast cancer patients typically receive this combination of treatments. This treatment effectively treats cancer while preserving more of the natural appearance and feel of your breast. According to research, lumpectomy plus radiation is nearly as effective at extending life as mastectomy (removal of a whole breast).
How is Lumpectomy Usually Done?
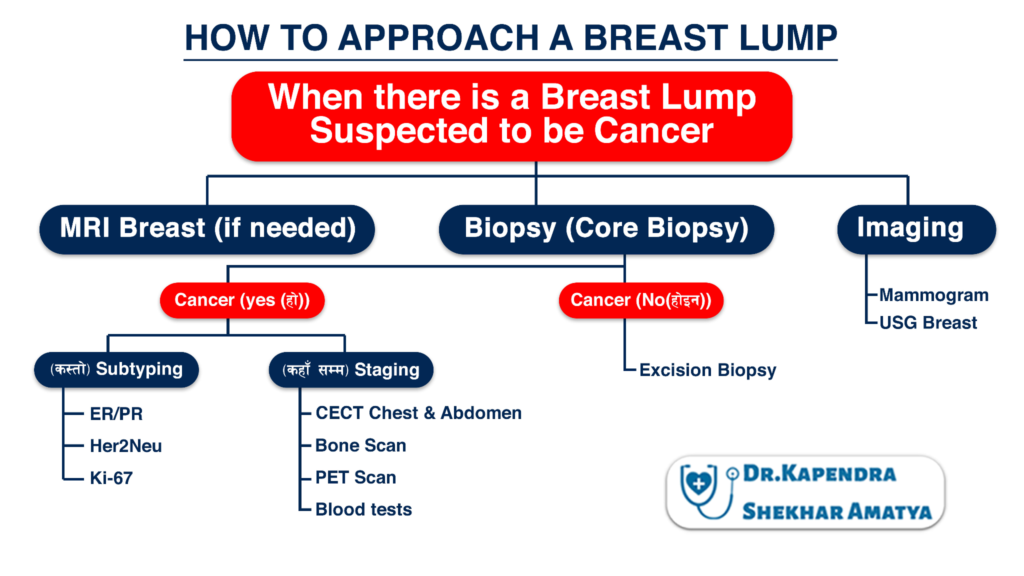
When we see a suspicious breast lump first question that arises is, Is this Cancer? Here we still rely of the triple assessment 1. Clinical Examination 2. Imaging: Mammogram, USG Breast, and if needed MRI Breast. 3. Tissue diagnosis: Core Biopsy (FNA as the last resort). This will give us the answer if the lesion is malignant or not. When diagnosed with Cancer, we further need to address two key issues.
1. What type of cancer it is? This is also called it subtyping; for this we rely on IHC for ER/PR, Her2Neu, Ki67.
2. Staging or Has the cancer spread?
a. How extensive is the cancer involvement within the breast?
The extent of cancer involvement within the breast is usually determined by the findings of the biopsy, the results of the mammogram, the ultrasound, and, in some cases, the results of the breast MRI scan.
b. Is there evidence that the tumor has moved to areas outside of the breast (metastasized)?
When these tumor cells lodge themselves in a lymph node (gland) or an organ such as the liver or the bones, they grow, eventually producing a mass or lump that can sometimes be felt or may only be evident because they cause symptoms such as bone pain and/ or can be seen on an imaging test such as a CT scan, a bone scan, or a positron emission tomography (PET) scan.
Patients usually go home the same day after lumpectomy surgery. Typically, the procedure lasts about an hour. The surgeon cannot see breast cancer, so the cancer is usually marked before surgery to assist in guiding them. The radiologist can insert a small chip or wire into the breast cancer to localize the cancer before surgery.
A lumpectomy involves removing the tumor and healthy breast tissue along with the tumor. In order to ensure that no cancer cells are left behind, surgeons leave a thin border of healthy breast tissue surrounding the tumor. To preserve your natural breast, providers remove only the tissue necessary to treat cancer. At the time of surgery, the pathologist and surgeon are unable to see the cancer. Therefore, determining the pathology results takes approximately seven to ten days.
To help reduce the amount of pain you will experience after surgery, your surgeon will probably administer pain medication to the surgical area. Additionally, the surgeon will place small marking clips at the site of the lumpectomy to assist the radiation oncologist. A dissolvable, internal stitch is then used to sew the breast tissue back together.
Consulting with Doctor for Lumpectomy Surgery
So as to go for the lumpectomy procedure, you must first consult with your oncologist thoroughly. You can either make an appointment with a surgical oncologist or a medical oncologist who will tell you everything in detail about your surgery. Your breast cancer oncologist will help you in each and every step during the entire surgical procedure. The breast cancer treating doctor can also help you deal with any additional side effects of the surgery.
What Happens Before The Lumpectomy Procedure?
Oncoplastic lumpectomy is a combined team approach surgery that enlists the help of a plastic/reconstructive surgeon in cases of large tumors. Unlike a traditional lumpectomy, an oncoplastic operation involves removing a larger piece of breast tissue and reshaping it to allow for better scar placement, nipple placement, and reshaping. To match the cancer breast size, oncoplastic surgery often involves reducing the volume of the other, normal breast as well.
Your healthcare provider will be able to tell you how your breast may change before surgery. You can discuss breast surgery options with your provider. To ensure your comfort, your provider will discuss procedure details with you before surgery. Whenever you have questions or concerns, ask your provider. Following your provider’s instructions, such as stopping certain medications before surgery, is important for your health and safety.
Your healthcare provider will be able to tell you how your breast may change before surgery. You can discuss breast surgery options with your provider. To ensure your comfort, your provider will discuss procedure details with you before surgery. Whenever you have questions or concerns, ask your provider. Following your provider’s instructions, such as stopping certain medications before surgery, is important for your health and safety.
What Happens After The Lumpectomy Procedure?
Recovery is the next step after your surgery. The blood pressure, pulse, and breathing of the patient will be monitored during this time. You’ll be released from the hospital when you’re in stable condition after outpatient surgery, usually a lumpectomy and a sentinel node biopsy. Having axillary lymph nodes dissected can result in pain or bleeding that requires a hospital stay for a few days.
Furthermore, you can also expect these:
• The surgical site is covered with a dressing
• A pinching sensation in your underarm area, as well as some pain, and numbness
• A written description of how to care for the incision and dressing after surgery and recognize signs of infection
• Possibly an antibiotic and pain medication prescriptions
• Restrictions on certain activities
• Usually seven to fourteen days after surgery, you will need to see your doctor for a follow-up appointment.
Possible Risk Factors of Lumpectomy
There are certain risks associated with lumpectomy, as with any surgery:
• Seroma: Following surgery, a seroma form when tissue was removed by the surgeon. It is sometimes necessary to drain a large amount of fluid.
• Infection: It is possible for the incision site to become infected. The skin can be infected with cellulitis in rare cases.
• Sensation loss: After a lumpectomy, part of the breast may become numb or lose sensation, depending on the size of the lump removed. Over time, the feeling may return in part or in full.
• Other cosmetic changes such as scarring, indentation, and dimpling: The healing of the skin can lead to cosmetic changes following a lumpectomy.
• Inconsistency in breast size: Following surgery, your breasts may be different sizes and shapes. A lumpectomy can result in a smaller breast. It’s possible that you don’t notice this right away because swelling can temporarily increase the size of your breast after surgery. Affected breasts can also be resized with radiation therapy.
• Pain in the nerves: A burning or shooting sensation may occur in the arm, armpit, or chest wall after surgery. This typically goes away in a few weeks or months. It is possible for nerve pain to last for a long time.
• Lymphedema: Lymphedema may develop if underarm lymph nodes are removed by the surgeon. When lymph fluid builds up in the arms, hands, or upper body, swelling can occur.
How to Get Prepared for Lumpectomy Surgery?
Here are certain preparation tips you can consider for your lumpectomy surgery:
• Don’t take aspirin or other blood thinners: The doctor may recommend discontinuing it at least a week prior to surgery in order to reduce bleeding risks.
• Consult your insurance provider: If you are going to have the procedure done at an outpatient facility, to determine whether it is covered and whether restrictions apply, contact your insurance provider.
• Avoid eating or drinking 8 to 12 hours before surgery: It’s best to avoid eating or drinking 8 to 12 hours before surgery, especially if you’ll be under general anesthesia.
• Bring a friend or family member: It may take several hours for the effects of anesthesia to wear off, so another person needs to drive you home and listen to postoperative instructions.
When Can You Get Your Results?
It should take a few days to a week for the results of your procedure to be available. The results of your surgery will be discussed with your doctor at your follow-up appointment. The following may be recommended by your doctor if you need more treatment:
• If the margins around your tumor were not cancer-free, your surgeon would discuss more surgery
• In addition to surgery, your medical oncologist may recommend hormone therapy, chemotherapy, or a combination of both after the operation.
• Typically, radiation treatment is recommended after lumpectomy, so an oncologist can discuss the options
• If you are dealing with breast cancer, you may benefit from counseling or a support group.
What to wear after lumpectomy surgery?
Wearing a crop top or sports bra might feel more comfortable until the swelling goes down. You will need to wear a supportive bra in the hospital after your surgery and when at home.
Some hospitals recommend wearing a bra all the time in the first few weeks. This can help to support the breast and reduce bruising.
If you wear a bra, it should be well-fitted and supportive. You should wear it during the night, for 1 week. You will probably be able to go back to work or your normal routine in 1 to 3 weeks after the surgery. This may depend on whether you have more treatment.

MS (NMC Regd.2902)
Head of the Department, Sr.Consultant Surgical Oncologist at Nepal Cancer Hospital and Research Center
Director: Breast Cancer Program
Interest: Breast Cancer Surgery, Gastro Intestinal Cancer Surgery (Stomach and Colo-Rectal Cancer)


