Table of Contents
ToggleDuring a mastectomy, a breast and surrounding tissues are surgically removed. In the past, breast cancer was treated with a radical mastectomy, which involved removing the entire breast, the lymph nodes under the arm, and some muscles underneath the breast. Surgical advances, however, have made it possible for people to have more choices. Many women can undergo breast-conserving treatments that are less invasive. You should consider several factors before choosing a type of mastectomy, including:
• An individual’s age
• The general health of an individual
• A woman’s menopause status
• The size of the tumor
• The extent of the tumor’s spread
• The aggressiveness of the tumor
• Status of the tumor’s hormone receptors
• The involvement of lymph nodes.
Why Mastectomy?
In cases of breast cancer or a high risk of developing it, a mastectomy is used to remove all breast tissue. Mastectomy can be done unilaterally or bilaterally to remove one or both breasts. Breast cancer may be treated with a mastectomy instead of a lumpectomy and radiation if:
• Breasts with two or more tumors.
• A breast biopsy revealed widespread calcium deposits that appear malignant in your breast.
• A previous radiation treatment to the breast region resulted in a recurrence of breast cancer.
• When you’re pregnant, radiation puts your unborn child at risk.
• cancer has been removed from the breast after a lumpectomy, but it remains at the edges of the operated area. There is a concern that cancer has spread to other parts of the breast as well.
• It is likely that you will develop a second breast cancer if you carry a gene mutation.
• As a percentage of your breast size, the tumor is large. An acceptable cosmetic result may not be possible after a lumpectomy due to insufficient healthy tissue remaining.
• The side effects of radiation to the skin may not be tolerated by patients with connective tissue diseases, such as scleroderma or lupus.
Types of Mastectomy:
Based on the method and extent of tissue removal, mastectomies are classified into different types. They are as follows:
Simple Mastectomy:
Surgery to reduce the breast involves removing the entire milk duct and pectoralis major fascia, along with the nipple and areola. In some cases, a sentinel lymph node biopsy may involve the removal of a few underarm lymph nodes. A majority of women can return home the next day if they are hospitalized.
Modified Radical Mastectomy:
There is a complete removal of the breast. There are three parts to the chest lining: the nipple, the areola, and the overlying skin. Additionally, some lymph nodes are removed under the arm. These lymph nodes are often affected by breast cancer. There is a possibility of it spreading to other parts of the body. Some patients have their chest wall muscles removed as well.
Radical:
In addition to the nipple, the areola, and the overlying skin, lymph nodes are removed under the arm. The chest muscles are also removed under the breast. Historically, this has been the standard surgery. However, it is rarely practiced today. Occasionally, breast cancer spreads to the chest muscles and this treatment is advised.
Skin-sparing:
There is a removal of breast tissue, the nipple, and the areola. There is, however, a significant amount of skin left over the breast. There is no evidence that this type of surgery works better than radical mastectomy. In the case of breast reconstruction following a mastectomy, this technique is only used. Large or near the surface of the skin tumors may not be appropriate for this method.
Nipple-sparing:
A similar procedure to the skin-sparing mastectomy is performed here. Some people refer to it as a total skin-sparing mastectomy. It involves removing the entire breast, including the ducts that run from the nipple to the areola. However, the skin of the nipple and areola remains intact. An expert called a pathologist carefully cuts away the tissue around the nipple and areola. There is a possibility of saving the nipple and areola if no cancer cells are found nearby. It is not recommended to use this method in any other case. After a mastectomy, reconstruction is performed.
Who Should Get Mastectomy?:
Breast conservation surgery (BCS) is a common option for women with early-stage cancer. A mastectomy may be your best option for removing all cancer as soon as possible. Nevertheless, mastectomy is not more likely to improve long-term survival than BCS in most cases. The outcome of BCS in conjunction with radiation has been shown in hundreds of studies over the past two decades to be similar to that of a mastectomy. You might need a mastectomy if you:
• Ineligible for radiation therapy
• A more extensive surgery would be preferred instead of radiation therapy
• An enlarged tumor, or a tumor larger than your breast size, of more than 5 cm (2 inches) in diameter
• Having inflammatory breast cancer.
Risk Factors for Mastectomy:
During any surgery, there is a possibility of bleeding and infection at the site. There might be a variety of side effects associated with different types of mastectomy. The following factors can increase your risk: • Tenderness or pain following surgery
• The area around the surgery site is swollen
• Blood accumulating in the wound
• An accumulation of clear fluid in the wound
• A limited range of motion in the arms or shoulders
• Upper arm or chest numbness
• The chest wall, armpits, and/or arm are painful and don’t go away after a while
• Lymphedema may result from removing axillary lymph nodes as well.
Consulting with Doctor for Mastectomy Surgery:
Before beginning your mastectomy procedure, you must have a thorough talk with your oncologist. You can either talk with a surgical oncologist or a medical oncologist who will tell you everything in detail about your surgery. The breast cancer oncologist will additionally help you with everything possible during the entire surgical procedure. Your breast cancer treating doctor can also help you reduce the additional side effects of the surgery.
How to Prepare Yourself for Mastectomy?
If you have any restrictions before surgery, you’ll be told what they are, as well as other things you should know, such as:
• Medications, vitamins, and supplements you take should be disclosed to your doctor: It is possible that some substances could interfere with the surgery.
• Taking blood thinners such as aspirin or ibuprofen should be stopped: You should talk to your provider a week or more before surgery about medications you should avoid avoiding excessive bleeding. Pain relievers like aspirin, ibuprofen, and warfarin, and blood thinners such as aspirin, belong to these categories.
• Eight to 12 hours before surgery, avoid eating or drinking: Your medical team will provide you with specific instructions.
• Be prepared for a hospital stay: Your doctor will be able to tell you how long you will be in the hospital. It would be helpful if you brought a robe and slippers with you to the hospital so that you could be more comfortable. Make sure you pack your toothbrush and a book to pass the time.
What Happens Before Surgery?
When you arrive at the hospital, your doctor or nurse will let you know. In most cases, a mastectomy without reconstruction can be performed in one to three hours. Many people go home the same day after their surgery, which is typically performed as an outpatient procedure. You may need to spend an additional day in the hospital if you are having both breasts removed. You may have to stay in the hospital for a few additional days if you’re having breast reconstruction following a mastectomy.
What Happens After Mastectomy Surgery?
You can expect to experience the following after your surgery:
• During your recovery room stay, your blood pressure, heart rate, and breathing will be monitored
• Dress the surgical site with a dressing
• An underarm area that feels numb, painful, and pinching
• Instructions on how to care for yourself at home, such as how to care for your incision and drains, how to recognize signs of infection, and what to do if you become ill
• Wearing a bra or wearing a breast prosthesis should be discussed with your healthcare team.
• Possible antibiotics and pain medications will be prescribed.
When Do You Get The Results and What You Should Do?
It shouldn’t take more than a week or two after your mastectomy for your pathology report to be available. You can discuss the report with your doctor at your follow-up visit. Your doctor may refer you to the following if you need more treatment:
• A radiation oncologist: In cases where a large tumor, many lymph nodes that tested positive for cancer, cancer that has spread into the skin or nipple, or cancer that remains after mastectomy, radiation treatments may be recommended.
• A medical oncologist: The doctor can discuss other treatment options after the operation, such as hormone therapy or chemotherapy if your cancer is sensitive to them
• A plastic surgeon: If you’re thinking about reconstructing your breasts.
• A counselor or support group: To assist you in coping with breast cancer
Q: What is a mastectomy?
A: A mastectomy is a surgery to remove the whole breast when someone has breast cancer or wants to reduce their risk of getting breast cancer.
- Q: How is a mastectomy done?
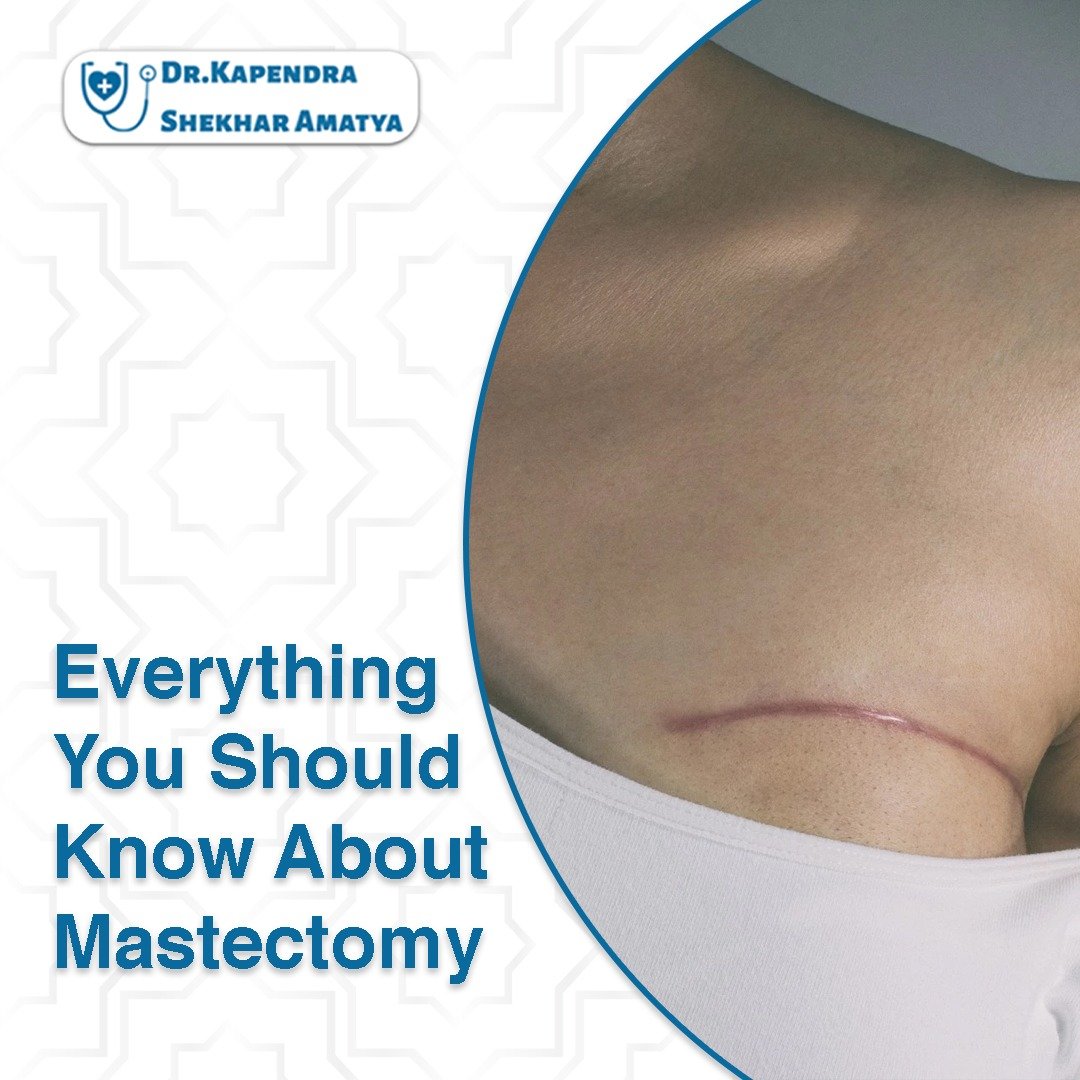
A: During a mastectomy, the doctor makes a cut on the breast and takes out all the breast tissue. Sometimes they also remove some nearby lymph nodes. The cut is then closed with stitches or staples.
- Q: Why do people have mastectomies?
A: People have mastectomies for different reasons. It can be to treat breast cancer that can’t be treated with other methods, to reduce the chance of getting breast cancer, or if there are multiple tumors in the breast.
- Q: What happens after a mastectomy?
A: After a mastectomy, the person needs time to recover. They might feel sore and swollen, but the pain can be managed with medicine. Physical activities may be limited at first, but gradually they will be able to move and exercise more. Sometimes, people choose to have breast reconstruction to make a new breast shape.
- Q: What are the risks and complications of mastectomy?
A: Like any surgery, there are some risks and possible problems after a mastectomy. These can include bleeding, infection, fluid buildup, or changes in sensation. It’s important to talk to the doctor about any concerns.
- Q: How does a mastectomy affect someone in the long term?
A: After a mastectomy, most people can live normal, healthy lives. The risk of the cancer coming back is often reduced. It’s important to have regular check-ups and tests to make sure everything is okay.
FAQ

MS (NMC Regd.2902)
Head of the Department, Sr.Consultant Surgical Oncologist at Nepal Cancer Hospital and Research Center
Director: Breast Cancer Program
Interest: Breast Cancer Surgery, Gastro Intestinal Cancer Surgery (Stomach and Colo-Rectal Cancer)


1 thought on “Everything You Should Know About Mastectomy:”